عرض هذه الصفحة باللغة العربية
Pancreatic cancer screening - Arabic
查看此页面的简体中文版本
Pancreatic cancer screening - Mandarin
Xem trang này bằng tiếng Việt
Pancreatic cancer screening - Vietnamese
Pancreatic cancer screening for people at increased risk
If you have a strong family history of pancreatic cancer or a genetic condition that increases your risk, regular monitoring may help detect abnormalities earlier and lead to better outcomes.
To understand whether you may be at increased risk, speak with your doctor or a genetic counsellor. They can review your family history and may recommend genetic testing. You can also take a short online quiz developed by Pankind: Pancreatic Cancer Australia or contact us at [email protected]u for more information.
People who are found to have a higher-than-average risk may be eligible to take part in the APRISE Study. This national research study offers yearly screening using MRI or endoscopic ultrasound. Details on eligibility criteria are provided below.
For more information or to join APRISE
For more information or to join APRISE, please contact us at 0418 370 684 or email
[email protected]
For health professionals, click below to refer your patient.
The APRISE Study is now open for enrolment
The Australian Pancreatic high-Risk ScrEening (APRISE) Study is a national research study led by the Jreissati Pancreatic Centre at Epworth in partnership with Pankind: Pancreatic Cancer Australia. The study is assessing whether regular screening can help detect pancreatic cancer earlier in people with a higher-than-average risk.
Screening in this study includes:
- A yearly MRI (magnetic resonance imaging) or EUS (endoscopic ultrasound) scan
- A brief yearly questionnaire about your health and medical history
You may be eligible for the APRISE Study if you fall into one of these high-risk groups:
- Are aged ≥ 18 and ≤ 90 years old
AND
- Without medical history of pancreatic cancer
AND
- Meet ANY of the following criteria:
- Familial Pancreatic Cancer Group 1
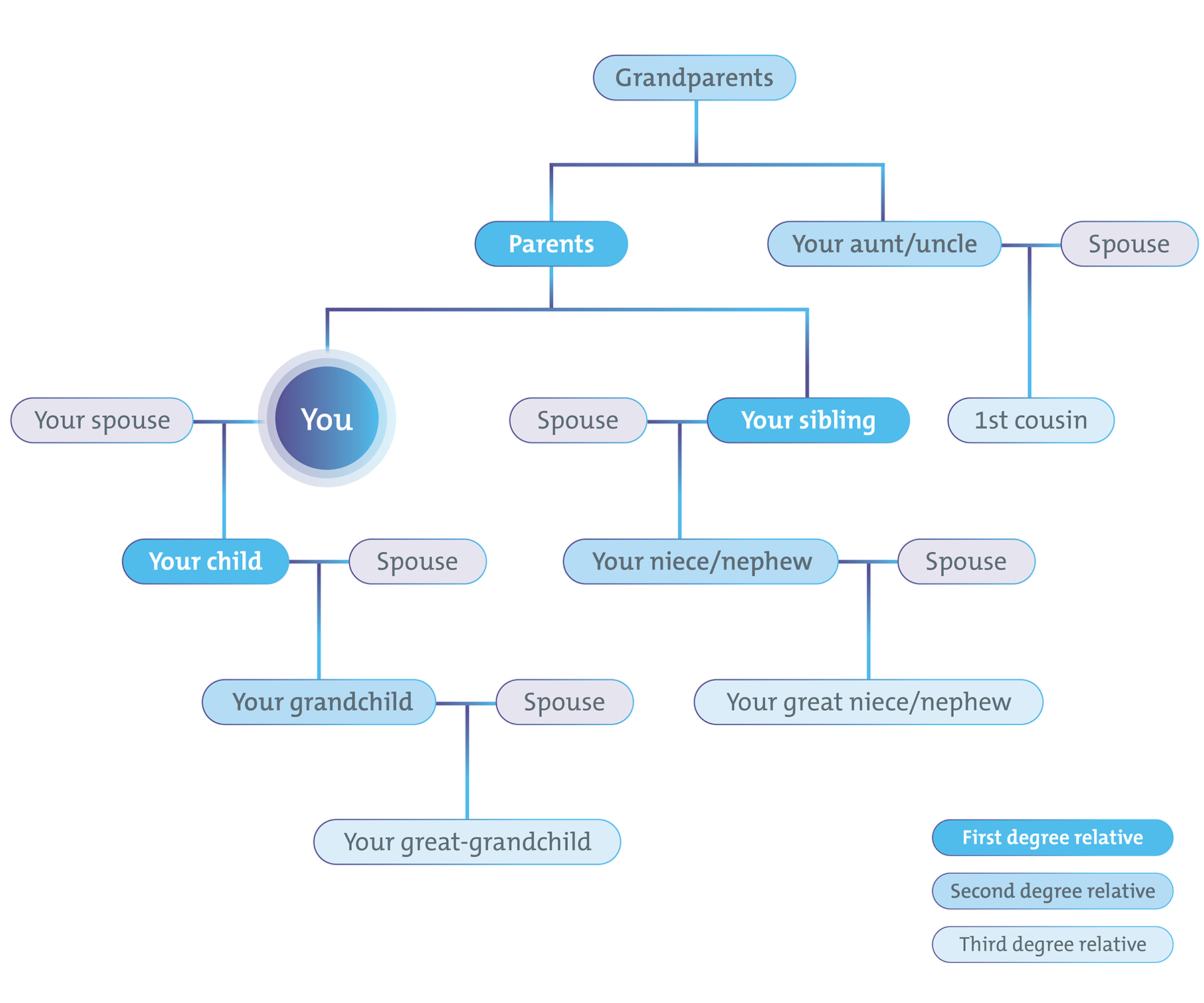
- ≥2 relatives with pancreatic cancer, on same side of family, where the 2 affected are first degree related to each other
AND - ≥ 1 affected is first degree related to participant
AND - ≥50 years of age, or 10 years younger than earliest pancreatic cancer in family at time of diagnosis.
- Familial Pancreatic Cancer Group 2
- ≥2 affected first degree relatives with pancreatic cancer
AND - ≥50 years of age, or 10 years younger than earliest pancreatic cancer in family.
- Pathogenic Variants
- BRCA1, BRCA2, PALB2, ATM, MLH1, MSH2, MSH6, PMS2, or EPCAM pathogenic or likely pathogenic variant
AND - 1 first or second degree relative with pancreatic cancer
AND - ≥50 years of age, or 10 years younger than earliest pancreatic cancer in family.
- Familial Atypical Multiple Mole Melanoma Syndrome (FAMMM)
- Familial Atypical Multiple Mole Melanoma (FAMMM) with pathogenic or likely pathogenic CDKN2A variant
AND - ≥40 years of age.
- Peutz-Jeghers Syndrome
- Peutz-Jeghers syndrome with STK11 pathogenic or likely pathogenic variant
AND - ≥35 years of age.
- Hereditary Pancreatitis
- Hereditary pancreatitis with PRSS1 pathogenic or likely pathogenic variant
AND - history of pancreatitis
AND - ≥40 years of age, or 20 years after onset of pancreatitis (whichever is earlier).
Take a quick quiz to see if you’re at risk
About 10% of pancreatic cancers are hereditary. If you’re unsure whether your family history puts you at increased risk, Pankind has developed a quick online tool to help.
Pankind Family Risk Checker
The Pankind Family Risk Checker is a short, interactive tool that takes about 3 minutes to complete.
By answering a few simple questions about your family history, the tool can help assess whether you may be at higher risk of developing pancreatic cancer. If you are potentially high risk, the tool will also guide you on next steps.
Where can I take part?
The APRISE Study is running at hospitals across Australia.
You can view the full list of hospitals below or check the map for a location near you. Please contact us at [email protected] for more information on how to access screening at these sites.
ACT
NSW
QLD
SA
|
TAS
VIC
WA
|
Frequently asked questions (FAQs)
Learn more about the APRISE program in our interview with Inherited Cancers Australia
-
About the study
Who is the study for?
This study is for people who may be at increased risk of developing pancreatic cancer due to family history or known genetic conditions. You do not need to have symptoms to take part. We can help check if you meet the eligibility criteria.
What are the benefits of taking part?
You may benefit from early detection of any problems with your pancreas. You will also be contributing to research that could improve screening and outcomes for others in the future.
How long will I be in the study?
You will be invited to take part in annual screening for several years, as long as you remain eligible and want to continue.
Will my information be kept private?
Yes. Your personal and medical information will be stored securely and managed in line with Australian privacy laws. Any research data will be de-identified before use.
-
Screening process
Do I need a referral?
Yes, a referral from your GP or specialist is required.
You can either:
- Contact us first at [email protected] and we can assess your eligibility. If you are eligible, we’ll let you know which hospital site to go to and who to get a referral to; or
- Go directly to a hospital site listed above. In that case, you’ll need a referral to the doctor listed for that site. Please ensure your GP referral letter references the APRISE study.
What is involved in screening?
Screening checks your pancreas for early signs of changes or problems, using one of two types of scans:
- Magnetic Resonance Imaging (MRI): This is a painless scan that uses magnets and radio waves to create detailed images of your pancreas. You will lie on a table that slides into a tunnel-shaped machine. The scan usually takes 30 to 60 minutes. It does not use radiation.
- Endoscopic Ultrasound (EUS): This test is done under light sedation. A thin, flexible tube with a small ultrasound probe on the end is passed through your mouth and into your stomach. This allows the doctor to take very detailed images of your pancreas from inside the body. Most people go home the same day.
The type of test you have will depend on what is most suitable for your medical history and what is available at the hospital site closest to you.
What happens after the screening test?
If nothing unusual is found, you will continue with yearly screening.
If something is detected, your doctor will explain the results and organise any follow-up tests or treatment. Your care will follow standard medical guidelines.
How often will I be screened?
Screening is done once a year to begin with.
If the screening test shows something unusual, you may need additional tests or more frequent follow-up. Your care will be based on standard clinical guidelines and tailored to your needs.
-
Costs and access
Is there a cost to participate in the study?
There is no cost to take part in the study itself.
However:
- You will need a referral from your GP or other health professional such as a genetic counsellor, which may involve a standard consultation fee if not bulk billed.
- If you choose to attend a private hospital, there may be out-of-pocket costs. These are not covered by the study and depend on your private health insurance and the specialist’s fees.
Do I have to pay for the screening tests?
It depends on whether you are seen in the public or private hospital system.
- Public hospital: Screening tests and appointments are fully covered by Medicare, so there is no cost to you.
- Private hospital: Medicare may cover part of the cost, but there may be an out-of-pocket fee depending on your cover and the specialist’s fees.
Do I need private health insurance?
No. You can take part in the study through either the public or private system. Private health insurance is only needed if you prefer to attend a private hospital.
Can I take part if I’m already being followed by a specialist?
Yes, possibly. Please contact us and we can check if you're eligible and how the study might align with your current care.
Resources for Health Professionals
APRISE fact sheet
APRISE eligibility criteria
For more information or to join APRISE
For more information or to join APRISE, please contact us at 0418 370 684 or email
[email protected]
For health professionals, click below to refer your patient.
This study is proudly funded by the Epworth Medical Foundation, Pankind: Pancreatic Cancer Australia, the Viridian Foundation, the Janko Inge Foundation, individual generous donors, and the Victorian Government through the Victorian Cancer Agency.